Vaccines Safety During Accelerated Research and Development
Posted on: Thursday 12 November 2020
Author: Penny Ward FFPM
This article has been prepared by Penny Ward FFPM.
It is provided for information and does not constitute advice or represent official FPM views or policy.
How to cite:
Ward, P (2020), ‘Vaccines Safety During Accelerated Research and Development’, Journal of the Faculty of Pharmaceutical Medicine, 10 November 2020. Available at: https://www.fpm.org.uk/journals/vaccines-safety-during-accelerated-research-and-development/ (Accessed: <date>).
Introduction
The 25 August 2020 certification of Africa as wild polio free1 serves to remind us of the value of vaccination in preventing infection related death and disability within populations. Vaccines are typically administered to healthy persons (including infants), therefore tolerance for adverse effects from vaccination is typically lower than tolerance to risks associated with medicines given to ill persons. Where sustained high coverage with an efficacious vaccine has led to near elimination of the target disease within a population, safety concerns can become even more prominent since fewer and fewer persons have experienced the disease but many persons will still be immunized and may be harmed. Rigorous scientific safety data are needed to optimize a vaccine’s benefit-risk ratio. In a public health emergency, the urgent need for an effective vaccine must be balanced against potential for vaccine related harms to ensure appropriate use. How can this be achieved when developing a vaccine at ‘warp speed’?
Vaccine Safety Evaluation: Learning from Experience
| Vaccine Strategy | Vaccine (human) | Advantages | Disadvantages |
|---|---|---|---|
| Inactivated vaccines | Influenza | Easy to prepare; safety; high titre neutralising antibody | Limited immune response in immunosuppressed/elderly |
| Attenuated virus vaccines | Oral polio, measles mumps and rubella (MMR), yellow fever | Rapid development; induce high immune response (humoral and mucosal) | Pheno/genotypic reversion potential; may cause (mild) disease |
| Subunit vaccines | Influenza | Safety; high titre antibodies; cellular and humoral response; consistent production | High cost; lower titre antibodies requiring adjuvants or repeated doses; |
| Virus like particle/Viral Vector | Ebola virus, Hepatitis B | Safety; high response (humoral and cellular) | Requires identification of antigens with neutralizing epitopes from recovered cases; effect and repeat use may be inhibited by pre-existing antibody vs viral vector |
| DNA vaccines | Zika, Dengue, Hepatitis B/C vaccines in clinical trials | Simple to design; high safety; high titre antibodies | No currently licensed vaccine in human use; delivery issues; toxicity risk (DNA insertion into human genome; anti DNA antibody stimulation) |
| RNA vaccines | Ebola Virus | Simple to design; adaptable; induce strong immune response | No currently licensed vaccine in use in humans/animals; stability; scale up limitations; unintended immunogenicity vs vaccine; potential autoimmune disease |
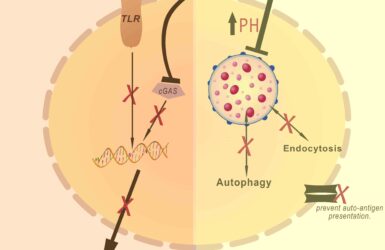
Advantages of using existing approved technologies in a pandemic emergency are multiple: established techniques result in availability of reliable manufacturing centres for rapid scale up; vaccine manufacturing components, including well qualified cell banks used for the initial viral culture (which have been built up since the recognition of vaccine contamination by several adventitious agents in the past2), are likely to be available for immediate exploitation; lastly, a great deal is known about the reliability of immune response to vaccines of this type, supporting extrapolation of existing knowledge to the new virus. In contrast novel techniques must start de novo and the manufacturing capacity built ‘at risk’3,4. In addition, performance of vaccines made using these technologies is not widely understood in practice, limiting ability to extrapolate from prolonged experience. Additional safety considerations may arise. For DNA vaccines, concerns include the development of autoimmunity, host cell genome integration and tissue destruction due to cytotoxic responses. There is also a potential concern for release of DNA products into the environment and other considerations linked to use of a genetically modified organism (GMO) in clinical practice5. The manufacturing processes for RNA vaccines do not require toxic chemicals or cell cultures that could be contaminated with adventitious viruses and, unless delivered within a viral vector, avoid the common risks associated with other vaccine platforms. The short manufacturing time required reduces the risk of introducing contaminating microorganisms and potential integration of the vector genome into host cell DNA is not a concern6. These features suggest RNA vaccines have some advantages relative to other technologies but also a potential risk regarding B cell activation and of exacerbating autoimmune reactions in some cases.
Preclinical Assessment
As for any new therapeutic, preclinical assessment must be completed prior to conducting clinical trials. The International Coalition of Medicines Regulatory Authorities (ICMRA) held several workshops to agree a consistent approach to vaccine development for COVID-19. FDA has also published regulatory guidance for this indication 7,8. Where adequate information to characterize product safety is available, e.g. the COVID-19 vaccine candidate is made using a platform technology utilized to manufacture a licensed vaccine or other previously studied investigational vaccines and is sufficiently characterized, it may be possible to use toxicology data and clinical data accrued with other products using the same platform to support FIH clinical trials with the new vaccine candidate. Local tolerance information with the candidate is required. Biodistribution studies in an animal species are required if the vaccine construct is novel, there is a likelihood of altered infectivity and tissue tropism or a novel route of administration/formulation is to be used. An immune response must be demonstrated in an in vivo animal model. A range of COVID-19 animal models have been investigated, each of which reflects different features of COVID-19 disease in humans. Although murine models are usually preferred (low cost, high reproductive rate and wealth of available reagents) wild type mice are unsuitable due to receptor incompatibility. A transgenic mouse model incorporating the human ACE2 receptor has been developed. Because hamster and transgenic mouse models display clinical symptoms these models have been used to study the early efficacy of various vaccines, while later studies (used to predict doses and safety assessments prior to human trials) have frequently been performed in non-human primates9-13.
Clinical Evaluation
The clinical development of vaccines follows that required for any therapeutic i.e. early studies in healthy volunteers to explore dose response (immunogenicity) and initial adverse effects and local tolerability, extending later to trials in vulnerable populations and large phase III programs to document prevention of infection/disease during a community disease outbreak and to continue vaccine safety assessment. To date, at least 41 candidate vaccines for SARS-CoV-2 have started clinical trials, of which 10 are in phase III, with 151 in preclinical testing20. Results of early trials have suggested vaccine associated adverse events (VAERs) include injection site reactions and systemic symptoms including fever, myalgia, joint pain, fatigue and headache at doses which result in satisfactory evolution of humoral and T cell immune response21-23. Safety evaluation of successful phase III candidates will need to continue post marketing. The Coalition for Epidemic Preparedness Innovations (CEPI) has funded the Brighton Collaboration to produce specific templates for standardised collection of COVID-19 vaccine associated adverse effects24 while WHO has enhanced the Global Vaccines Safety Initiative (GVSI)25. In the EU, surveillance will be enhanced by the ADVANCE consortium, which was formed after the late recognition of an increased risk of narcolepsy caused by a licensed pandemic influenza vaccine26. The stage is set: we await arrival of the first SARS-CoV-2 vaccine(s).
References
- WHO News Release: Global polio eradication initiative applauds WHO African region for wild polio-free certification. 25 August 2020.
- Petricciani J, Sheets R, Griffiths E and Knezevic I. Adventitious agents in viral vaccines: Lessons learned from 4 case Studies. Biologicals (2014); 42: 223e236
- Smith J, Lipsitch M and Almond JW. Vaccine production, distribution, access and uptake. Lancet (2011); 378: 428–438.
- Plotkin S, Robinson JM, Cunningham G, Iqbal R and Larsen S. The complexity and cost of vaccine manufacturing – An overview. Vaccine (2017); 35: 4064-4071
- Myhr AI. DNA Vaccines: Regulatory Considerations and Safety Aspects. Curr. Issues Mol. Biol (2017); 22: 79-88.
- Pardi N, Hogan MJ, Porter FW and Weissman D. mRNA vaccines — a new era in vaccinology. Nature Reviews Drug Discovery (2018); 17: 261-279.
- International Coalition of Medicines Regulatory Authorities (ICMRA) Workshop Reports March 2020, June 2020 http://www.icmra.info/drupal/en/covid-19
- FDA Guidance Document: Development and Licensure of Vaccines to Prevent COVID-19 Guidance for Industry JUNE 2020. https://www.fda.gov/media/139638/download Accessed 1 September 2020
- Lakdawala SS and Menachery VD. The search for a COVID-19 animal model. Science (2020); 368: 942-3.
- Yahalom-Ronen Y, Tamir H, Melamed S, Politi B, Shifman O et al. A single dose of recombinant VSV-∆G-spike vaccine provides protection against SARS-CoV-2 challenge. BioRxiv (2020); https://www.biorxiv.org/content/10.1101/2020.06.18.160655v1
- van Doremalen N, Lambe T, Spencer A, Belij-Rammerstorfer S, Purushotham JN et al. ChAdOx1 nCoV-19 vaccination prevents SARS-CoV-2 pneumonia in rhesus macaques. BioRxiv (2020); https://doi.org/10.1101/2020.05.13.093195
- Mercado NB, Zahn R, Wegmann F Loos C, Chandrashekar A et al, Single-shot Ad26 vaccine protects against SARS-CoV-2 in rhesus macaques, Nature (2020). DOI: 10.1038/s41586-020-2607-z
- Yu J, Tostanoski JH, Peter L, Mercado NB, McMahan K et al. DNA vaccine protection against SARS-CoV-2 in rhesus macaques. Science (2020); 10.1126/science.abc6284
- Wan, Y., Shang, J., Sun, S., Tai, W., Chen, J et al. Molecular mechanism for antibody-dependent enhancement of coronavirus entry. J. Virol (2020).; 94, e02015-19.
- Halstead S.B. Pathogenesis of dengue: challenges to molecular biology. Science (1988); 239: 476–481.
- Halstead SB, Katzelnick LC, Russell PK, Markoff L, Aguiar M et al. Ethics of a partially effective dengue vaccine: Lessons from the Philippines. Vaccine (2020); 38: 5572-5576.
- Vennema, H., de Groot, R.J., Harbour, D.A., Dalderup, M., Gruffydd-Jones, T et al. Early death after feline infectious peritonitis virus challenge due to recombinant vaccinia virus immunization. J. Virol (1990); 64: 1407–1409.
- Ruckwardt, T.J., Morabito, K.M., and Graham, B.S. immunological lessons from respiratory syncytial virus vaccine development. Immunity (2019); 51: 429–442.
- Bolles, M., Deming, D., Long, K., Agnihothram, S.,Whitmore, A et al. A double-inactivated severe acute respiratory syndrome coronavirus vaccine provides incomplete protection in mice and induces increased eosinophilic proinflammatory pulmonary response upon challenge. J. Virol (2011); 85: 12201–12215.
- WHO Draft landscape of COVID-19 candidate vaccines. https://www.who.int/publications/m/item/ draft-landscape-of-covid-19-candidate-vaccines. (Accessed 30 September 2020).
- Folegatti PM, Ewer KJ, Aley PK, Angus B, Becker S et al. Safety and immunogenicity of the ChAdOx1 nCoV-19 vaccine against SARS-CoV-2: a preliminary report of a phase 1/2, single-blind, randomised controlled trial. Lancet (2020); https://doi.org/10.1016/S0140-6736(20)31604-4
- Zhu FC, Li YH, Guan XH, Hou LH, Wang WJ et al. Immunogenicity and safety of a recombinant adenovirus type-5-vectored COVID-19 vaccine in healthy adults aged 18 years or older: a randomised, double-blind, placebo-controlled, phase 2 trial. Lancet( 2020); https://doi.org/10.1016/S0140-6736(20)31605-6
- Jackson LA, Anderson EJ, Rouphael NG, Roberts PC, Makhene M et al. An mRNA Vaccine against SARS-CoV-2 – Preliminary Report. N Engl J Med. 2020;10.1056/NEJMoa2026920. doi:10.1056/NEJMoa2026920
- Chen RT, Kochhar S, Condit RC The Brighton Collaboration standardized templates for collection of key information for benefit-risk assessment of vaccines by technology (BRAVATO; formerly V3SWG). Vaccine (2020); 38: 6184–9.
- World Health Organization. Global Advisory Committee on Vaccine Safety, 27–28 May 2020: Conclusion and recommendations. Wkly Epidem Rec 2020; 95: 336.
- Sturkenboom M, Bahri P, Chiucchiuini A, Grove Krause T, Hahné S et al. Why we need more collaboration in Europe to enhance post-marketing surveillance of vaccines. Vaccine (2019); S0264-410X(19)31002-3. doi:10.1016/j.vaccine.2019.07.081
More from the Autumn/Winter 2020 edition of the FPM Journal