FPM Clinical Trials Resilience Survey – Report Published
Posted on: Wednesday 16 December 2020
Author: FPM
Executive summary
The COVID-19 pandemic has disrupted the lives and livelihoods of many of the members of the Faculty of Pharmaceutical Medicine (FPM). In the UK, within both the NHS and national economy resources were diverted in an attempt to manage the outbreak. This effort was mirrored across pharmaceutical medicine, with pharmaceutical companies and regulators pausing or postponing the start of many trials in other disease areas to focus on the hunt for therapies for COVID-19.
This refocusing in approach has been enormously challenging, but we have learnt a lot over the last few months, and the return to the non-pandemic clinical trial landscape in the ‘new normal’ could be very different.
The FPM Clinical Trials Resilience Survey (Oct-Nov 2020) sought to understand these pressures and the adaptations that our members have experienced. We wanted to try to learn whether the COVID-19 pandemic has brought about permanent changes to pharmaceutical medicine and drug development and regulations that could or should now become integrated into ‘normal’ practice.
The results are illuminating and will help guide FPM and our external stakeholders as the current pandemic continues. The outputs from the survey may be relevant to maintaining effective systems during further COVID-19 waves, but also to future, as yet unknown, pandemics and global health challenges.
About the survey
Demographics
- The ‘Clinical Trials Resilience Survey’ was run by FPM between the 22nd October and the 4th November 2020
- The survey was sent to all 1500+ members of FPM and was also made available to non-members to complete
- FPM members are medically qualified and employed within the pharmaceutical industry, biotechnology companies and contract research organisations, or the drug regulatory authorities
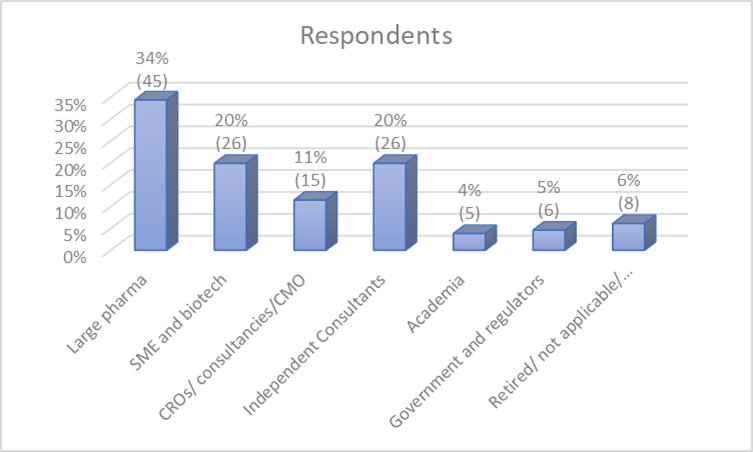
- 128 people responded, including 118 members and 10 non-members
- 75% (95) respondents were based in the UK / 9% (12) in USA / 9% (12) in Europe outside UK / 7% (9) from outside Europe and the USA
- The majority of respondents worked on clinical trials; 70% respondents stated they worked on clinical trials and drug development and 19% in clinical pharmacology and 11% did not record involvement in trials. Just over half worked in pharmaceutical companies and biotech companies and just under half in contract research organisations (CROs) / contract manufacturing organisations (CMOs) or as consultants
Adaptions made to expedite treatments or vaccines for COVID-19
Over half the respondents (54%) reported that their organisation has been directly involved in developing treatments or vaccines for COVID-19.
Those respondents that were involved in developing treatments or vaccines for COVID-19 reported on vaccine programmes, therapeutic antibodies, small molecules, stem cell treatments, palliative care and programmes for repurposing. Several respondents’ COVID-19 drugs were being developed at the expense of other programmes being put on hold.
The impact on non-COVID-19 clinical research programmes
79% of all respondents reported that other clinical research programme activities in their organisation had been impacted by the pandemic.
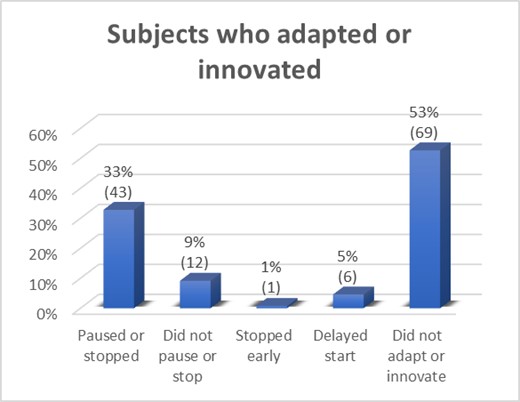
Inevitably, many respondents reported delays to trial programmes. One respondent working in a CRO noted that sponsors had shifted complete strategic focus and closed entire development programmes. Another CRO respondent reported the furlough of staff and refocusing on writing COVID risk assessments. Compounding factors were reported included delays in essential pre-clinical development and manufacturing. Lack of study feasibility visits resulted in preventing sites being set up and initiated and study start deferral was reported.
What adaptations and innovations have been made for non COVID Trials
Over half the respondents to this question reported no change to the designs of their development programmes. Of the remaining respondents; one reported having to drop one of their intended indications, one stated they re-focused on trials of lower risk molecules only, not those for autoimmune diseases or immunomodulation drugs; several (5) reported switching programmes to use remote monitoring and virtual meetings; and three switched ongoing programmes to COVID indications. Programme design as opposed to individual trials was reported to include focus on risk mitigation and contingency plans.
The impact of the pandemic on SOPs for clinical programmes and trial design
Almost half of respondents (48%) reported that the pandemic had impacted their organisation's standard operating procedures (SOPs) for clinical programmes and trial design and brought about variations to their Good Clinical Practice. A significant portion of those responding survey were already considering permanent changes to SOPs. We asked them to group their response to different categories.
General standard operating procedures (SOPs) have been written for issues such as global health security planning and re-prioritisation of programmes at global level. These SOPs extended to PPE, general hygiene and screening. Some respondents noted that the pandemic had impacted costs and the ability to raise money, sometimes easier and sometimes more difficult. The extension and adaptation of trials could also mean the companies might run out of money to complete the trials.
External examples of successful adjustments to clinical research & development
This section was for comments from the respondents on activities they had learnt about and had appreciated, but were not involved in.
Most of the research and development community were thought to be more collaborative, which was strongly welcomed. Some respondents were frustrated by a lack of overall unified and global leadership, that transcends country politics. Something that the pharmaceutical industry is used to through ICH. EFPIA support of increased collaboration across pharma/ academic/ regulators/ government bodies e.g. AZ/GSK/University of Cambridge lighthouse lab was thought to have been valuable.
Building resilience for the future
Most respondents (78%) stated that at least some of the changes to clinical programme design and operational practice brought about by the pandemic could be integrated into best practice moving forward and help to build resilience against potential further global pandemics and health challenges.
It was suggested that the pharmaceutical and biotech industries need stronger strategic senior engagement with CEOs and Medical Directors of hospitals, not just the local Principal Investigator and R&D department (who the members of FPM normally interact with), to build advocacy for the importance of commercial research. To emphasise the importance of clinical research at this time of the UK leaving the EU is important to all stakeholders. A thriving industry in the UK brings benefit to all.
One respondent thought that more clinical trial sites for non-COVID-19 trials need to have comprehensive business continuity plans and service level agreements, in the eventuality of another pandemic or other disasters.
It was suggested that more UK involvement in trials would benefit more Site Management Organisation (SMO) sites. This could be in the form of one hospital or GP practice, with a PI acting as a hub and distributing trial activities to other hospitals or GP practices, which could act as buffer when hospitals and GPs are overloaded. In this regard the NIHR as the overall broker could facilitate when using its staff in the Clinical Research Networks.
In the pandemic most trials were, from a national perspective, overseen by the NIHR and it was felt that it could have been valuable to have more decentralised trials. A second suggestion was that increased devolved trial models should make these more resilient to future pandemics or other disruption.
One respondent said that the NHS needs to be much better equipped and protected with PPE and frequent testing. COVID-19 (or any other contagious disease) free areas in hospitals need to be established to give subjects the confidence to come for appointments and forms of safe transport to appointments need to be created. This would mean existing non-COVID-19 trials would have a better chance of trials of continuing.
It was noted that the global pandemic preparedness deviated substantially from our historical ‘best practice’. It is becoming apparent that virology drug development has not been prioritised to an appropriate extent in the decade since last flu pandemic. This is a global issue and very few general antivirals, such as SNG001, have been brought into development. Support for general antivirals in drug development, rather than only vaccines, is required moving forward.
There is a perception that smaller companies with innovative products may have been overlooked by NIHR and other government funds, and that support was given to larger and often less innovative companies. It is easy to understand due the need for outside funding by the bigger companies, but could limit innovation at a time when many of the aspects of the disease had never been seen before and so presenting major scientific challenges. Other funding risks induced by COVID-19 include a diversion of funding from major charitable and academic funding bodies, which will have an impact on non-COVID-19 programmes.
Clear guidance and improved communications from the NHS and NIHR on a strategy for the restart of clinical trials and on which types of trials should be prioritized was requested. The non-COVID-19 trials that have been heavily impacted were not prioritized. One respondent suggested to ensure better remote eMR access across all NHS trusts should be a standard. Consideration of flexibility around standard of care procedures/tests to be performed by local GPs/hospitals where possible were thought to be something that might be helpful both in and outside clinical trials.
There was a request to engage with key external stakeholders (mainly governmental) to ensure that political leaders are educated appropriately in statistics and data interpretation and more importantly that the UK plans properly for future pandemics and has appropriate infrastructure, systems and processes in pace to deal with any situation that may arise.
Improving collaboration with government agencies worldwide on international healthcare initiatives would be helpful especially for big multicentre studies, whilst also helping in the integration of data, digital, diagnostic and pharmaceutical companies. The aim would be to achieve more global collaborations, with harmonized and joined effort in future clinical programmes.
Summary
We are very grateful to those who gave their time to complete the survey. The data and information gathered will help FPM and external stakeholders learn and develop and innovate in their plans and procedures. We hope that if/when a similar pandemic transpires the global community will be even better placed to combat that threat.
Risk planning for pandemics needs to be reviewed and updated for all activities related to clinical trials and pharmaceutical medicine. Much of what has come out of the pandemic will improve research and collaboration. Regulators and sponsors need to discuss future flexibility around all research procedures. Adoption of tools that can easily be adapted for remote use e.g. e-consent and remote monitoring / approval of apps to support trials should be encouraged, validated and enabled.
In order to embed resilience into the healthcare system, it is recommended that post-COVID-19, there must be more of a focus of attention and funding on infection, including targeted and non-targeted virologics, vaccines, antibiotics and antifungals. Also, a reminder that infection is the commonest respiratory disease and killer. This will allow us to be better prepared for the inevitable emergence of resistant pathogens whether they be virus, bacteria or fungi. Future pandemics will happen, but we must not ignore the regular significant mortality of seasonal disease patterns.
Small companies with innovative products and ideas should not be overlooked and should be engaged and incentivised to participate in collaborations and joint programmes.
A lack of relevant pharmaceutical medicine & medicines development expertise in decision-making positions within key stakeholders should be considered and this could help inform a re-prioritisation of clinical trial programmes at a global level, both within individual organisations and in collaboration. This would support a consolidated shift to global health security programming.
Recommendations
Throughout this report we have attempted to summarise and analyse the data we obtained, and here we make recommendations for four overarching groups:
- Centralised public sector bodies are encouraged to embrace all skill sets across professional groups related to vaccine and drug development, including those from industry
- Stronger links should be developed between industry, NIHR, Government, regulators and the medical directors of hospitals to ensure all trials are pandemic resilient
- There should be a research focus and associated funding on developing technology and safe standards for the remote conduct, monitoring and audit of clinical trials
- During a pandemic, regulators and national agencies should prioritise trial applications on a case-by-case basis, based on the broad public health benefit, transparency is key in this process
- During a pandemic, where appropriate, all stakeholders should develop communications to patients to inform, education and help to reduce anxiety regarding participation in new and ongoing trials
- A centralised system for the prioritisation of trials and the allocation of patients should be considered
- A national strategy for re-start of clinical trials should be developed.
- Consideration should be given to site management organisation through NIHR, to allow shifting of site visits or such things as taking biopsies, where the overload in one hospital exceeds another
