Principles for Clinical Studies into COVID-19
Posted on: Thursday 28 May 2020
Introduction
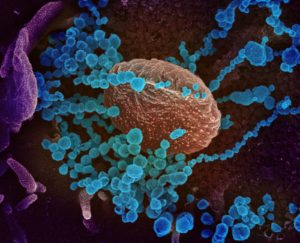
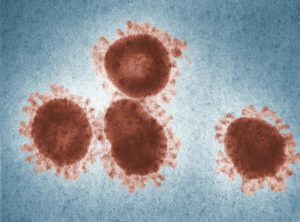
Since the emergence of the novel coronavirus SARS-CoV-2 and the World Health Organisation (WHO) declaration of a pandemic, there has been a rapid expansion in COVID-19 related clinical studies. These have been initiated by many different academic, commercial, governmental and health care sponsors to investigate disease control and to develop effective treatments.
While well intentioned, many studies are small, not well controlled and may not be able to deliver robust and interpretable results1. The ethical dimensions and opportunity cost of larger, well controlled or pooled studies cannot be ignored in terms of the individual patients enrolled.
The Faculty of Pharmaceutical Medicine, whose members are experienced in clinical study design, have developed these principles, for consideration by sponsors, investigators, ethics committees and journal editors.
How to cite:
Dollow, S et al. (2020), ‘Principles for Clinical Studies into COVID-19’, Faculty of Pharmaceutical Medicine blog, 27 May 2020. Available at: https://www.fpm.org.uk/blog/principles-for-clinical-studies-into-covid-19/ (Accessed: <date>).
Governance
- The COVID-19 pandemic and knowledge about its presentations is evolving rapidly, with many clinical trials being planned and conducted in abnormal circumstances. Haste should not however compromise participant safety or scientific integrity. Where there is a risk of infection, adequate safety procedures for isolation and use of protective equipment must be in place to protect staff and other patients / study participants. This should extend to consider others who may be secondarily exposed to participants who may be infectious.
- Sponsors must ensure that during the pandemic, supplies of investigational products and other necessary components will be available in sufficient quantities to complete the study and not compromise its conduct or integrity. Sponsors should ensure they consider the possibility of social restrictions being imposed that may restrict study visits and data collection. Protocols must include appropriate contingency plans to ensure studies remain viable and analytically robust and can recruit the sample size in a reasonable time.
- All trials should be conducted according to Good Clinical Practice (GCP)2 and be approved by a legally constituted ethics committee, prioritising participant safety at all times. In transmission studies, with or without deliberate infection or household exposure, if governmental guidelines on infection prevention may be contravened, there must be early engagement with the relevant regulatory authority. Any adaptations to GCP, made in exceptional circumstances, must be documented and approved by the governing ethics committees, and must include a full assessment of the ethics and benefit-risk of any deliberate infection and household exposure techniques within vaccine studies.
- Standard regulatory guidance should still apply. However the most recent COVID-19 related guidance from the regulatory authorities in the country where the study is planned must also be reviewed and the authorities consulted. FDA, EMA and MHRA have all provided specific guidance3, 4, 5 while WHO have provided ethical guidelines for SARS-CoV-2 human challenge studies6.
- Understanding of therapeutic interventions will continue to evolve, with the possibility of viral mutation, multiple waves of infection and new therapies being introduced during study conduct. As such, COVID-19 studies need to be reviewed regularly to ensure their ongoing suitability based on any emerging evidence, adjusting the ‘standard of care’ midway through a study if appropriate, or abandoning use of a placebo if it becomes unethical. Ethics committees must be consulted whenever material information from the trial or other studies emerges, and regularly updated during the conduct of the trial.
- All studies should be listed on a publicly accessible register with a firm commitment to share patient level data regardless of study outcome. This is required regardless of whether the intervention(s) are approved for other indications.
Consent
- All participants are expected to provide informed consent, based on a clear understanding of the risks, possible benefits and alternative therapies that may be used (whether fully licensed or not). Considerations for witnessed consent, gaining consent preserving isolation requirements and consent from incapacitated patients should be included and be in line with local regulatory and ethical guidance.
- Vaccine studies utilising human challenge or household exposure techniques, must clearly explain the risks of deliberate or other exposure to infection within the consent.
Study Design
- First in Human (FIH) / Phase 1 studies can be especially challenging during a pandemic. Participant safety remains paramount. Stopping rules, careful assessment of all adverse events and a Data and Safety Monitoring Board (DSMB) should all be in place. Importantly, even for repurposed medicines, First into Disease studies should be undertaken cautiously. Prior evidence of safety demonstrated in different indications is no assurance that the same safety profile will be exhibited in SARS-CoV-2 patients. The principles of a Phase 1 FIH study should be followed.
- The study design must be justified, based on a robust explanation and understanding of the preclinical science. Modelling and simulation should be used to maximise data utility from the minimum number of participants, and endpoints that are relevant to the mechanism, the disease and the phase of the study should be selected. The use of endemic coronavirus strains as practical surrogates in proof of concept vaccine studies should be considered.
- Given the likelihood of study disruption being high, with participants becoming unwell, or having to self-isolate at short notice, studies should not be unnecessarily complex. Designs that require institutionalisation for prolonged periods should be avoided.
- A COVID testing regimen should be in place, bringing participants in early to ensure they are uninfected. Participants should be dosed in small groups within a cohort with appropriate social distancing, to minimise the impact of incident infections. Healthy volunteers should be separately studied to minimise the risk of transmission.
- The possibility of changes in the standards of care that may impact the study, such as availability of a vaccine, must be considered in advance. Contingency plans to temporarily suspend and evaluate conduct, or prematurely terminate the study must be in place and involve the ethics committee and/or the DSMB.
- Efficacy and safety studies should include a robust statistical analysis plan within the protocol that compares the investigational agent(s) to a defined appropriate comparator or standard of care. Standard of care is also expected to be used as background therapy to the investigational agent with or without the addition of an alternative active therapy/placebo. The comparator group should ideally be randomised within the study, although comparators from a suitably matched external database or similarly designed study are acceptable if prospectively stated.
- 3rd party randomisation should be used to ensure that allocation bias is removed or minimised. Important patient factors should be balanced across treatment groups, using stratification and minimisation techniques.
- Wherever possible, double-blind studies are advised to minimise bias. The use of blinded study materials, double dummy or other techniques should be employed, together with independent allocation to, and administration of, the study intervention.
- Where this is not possible, single blind, or observer / independent blinded assessment of outcomes should be included within protocols. Prevention of infection for observers must be prioritised.
- Observational and safety studies must allow participants to follow local or national guidance on acceptable techniques for transmission prevention.
- Appropriate statistical analyses must be described in the protocol at the outset.
Standardisation of entry criteria
- COVID-19 disease has different presentations and stages. Studies range from pre and post exposure prophylaxis, through asymptomatic infection to the most severe presentations of acute respiratory distress syndrome (ARDS) and multiple organ failure. Patient studies should select, where appropriate to the study hypothesis and intervention, the most discrete stage of disease possible based on our emerging understanding of its progression.
- Patient selection criteria and end points should reflect existing accepted regulatory guidelines for the indication under study (e.g. viral transmission / ARDS).
- Within and across studies every effort should be made to standardise selection criteria to ensure that studies of different interventions at different stages of disease are comparable, generating meaningful information for prescribers on the patients in which it should be used. Protocols should define the eligibility criteria as closely as possible, without unduly excluding any particular patients or vulnerable groups. Patient comorbidities should be recorded for further analyses, notwithstanding the challenges of doing so in certain settings.
Therapeutic intervention
- The justification, plausibility and evidence to support the use of the investigational therapy should be described, together with PK/PD justification for the doses, frequency of administration, duration of treatment and exploration of the ranges of each.
- The relative strengths and weaknesses of the therapeutic approach, together with the relative merits of alternative approaches (that may be denied to patients by participation in the study) should be explained.
Evidence based end points and their duration
- The rationale for selection of the endpoints, based on the stage of COVID-19 pathology and the mechanism of action of the intervention under study should be justified.
- End points should be relevant to the aim of the study, reflecting existing regulatory guidance and should be validated or widely agreed as being appropriate (by groups such as COMET7) to allow for meta-analysis and cross study comparison.
- Use of biomarker endpoints should be explained in the context of the disease stage, mechanism of action of the product and potential link between the biomarker and a relevant clinical outcome. Where biomarkers are used as endpoints or for enrichment or stratification, patient follow-up to validate their use according to existing guidelines8 and to monitor the eventual clinical outcome must be included within the protocol.
Independent Adjudication
- Use of an independent, suitably experienced DSMB and an Independent Data Monitoring Committee (IDMC), operating to defined constitutions that include unblinding rules, should be considered and are strongly advised, especially in larger therapeutic studies. These roles may be combined into one independent body for smaller studies.
- IDMCs should be closely involved in the judicious use of interim analyses to provide guidance on areas such as adaptation of study designs, study repowering based upon changes to expected event rates, the validity of endpoints or emerging external data. Extreme caution should be exercised by IDMCs in any announcements of interim efficacy/safety results in advance of firm outcomes.
- DSMBs should be closely involved in ongoing review of safety or outcome data, particularly in studies of severely ill patients. Both IDMCs and DSMBs should have authority to recommend study amendments, including early termination or dropping of doses.
- Justification for not having a DSMB or IDMC in these studies should be given.
- To minimize harm to individuals and to allow appropriate action to be taken in the event of emerging data on benefit-risk, notwithstanding the uncertainties regarding the natural history of COVID-19 disease, stopping rules should be defined within the protocol and continually reviewed for suitability. Stopping rules should operate at the level of individual participants, patient cohorts and the study itself. In these cases, the plan for analysis of participant data collected to that point should be prespecified.
- Reviews of emerging study data and their trigger points (e.g. numbers of events) should be detailed in the protocol. The conditions of the review should be defined and should include the process of unblinding the DSMB, while maintaining the blinding of the investigators and sponsor, the potential impact on the statistical power of the study and mitigating actions taken to avoid bias as a result. Predefined threshold levels for taking resulting decisions should be included in analysis plans.
Statistical Considerations
- A statistical analysis plan should be written as appropriate for the phase of investigation. It must justify the sample size selected for the study and the intended analysis of the outcomes. The plan should be sufficiently advanced that it can be made available at the time of submission of the protocol for ethical and, where appropriate, regulatory approvals, if requested.
- Sample sizes should be based on a meaningful difference in the primary endpoint used. For pharmacodynamic outcomes, the sample size should be sufficient to take variation in the laboratory measure into account. For clinical endpoint studies, the minimal relevant clinical difference proposed should be justified within the context of variability in outcomes in various stages of disease. The sample size selected should be large enough to provide an appropriate level of confidence (α) and powered (β) sufficiently to provide robust evidence of effect.
- Platform/ adaptive trials intended to investigate multiple medications or combination treatments should be of sufficient size to enable valid conclusions at each step accounting for variability in endpoints from multiple interventions.
- Randomisation methods used should minimise potential bias, particularly where these result from variations in severity of disease at the time of randomisation, to avoid analyses providing misleading findings.
- Trial outcomes and endpoints should be relevant to the phase of the study and the intended use of the information obtained. Dependent on the study phase, suitable endpoints may include pharmacokinetic data, pharmacodynamic effects on biomarkers of disease and/or target engagement, viral replication or clinical outcomes. In turn, these will depend on the study intent and stage of disease among the patient group to be included and must be justified.
- Analysis of subgroups (e.g. according to medications received, patient characteristics or disease stage at trial entry) should be described and justified a priori within the statistical analysis plan.
Other studies
- To avoid duplicate or redundant studies, a justification of the utility of the study and whether similar work has already been conducted or is ongoing, must be included together with an explanation of what the study will add to the existing knowledge base. This should include expected next steps to perform confirmatory studies or further assessments required to bring the intervention into clinical use if the trial is positive.
- Investigators should explain why, when similar studies are planned or ongoing elsewhere, their study should proceed and what steps they have taken to collaborate with other investigators and sponsors to expand the sample size and reduce unnecessary patient exposure and risk.
- A commitment to making patient level data available should be present to enable pooling of information with data from other studies in similar patient populations.

Conclusion
Poorly designed, conducted and reported studies carry significant and unacceptable risks to the participants and the wider public. The data that emanates from them may be flawed and often take considerable effort to refute4.
Whilst current efforts are beginning to contribute significant benefits, we emphasise that studies should follow the best principles of clinical development to provide society with the best chance to rapidly develop evidence-based treatments for the various presentations and phases of COVID-19.
Building on the experience of setting up studies during the COVID-19 pandemic, together with broad agreement on principles such as these, should lead to an improvement in study consistency and robustness of evidence to improve the investigation and clinical management of this and future public health emergencies.
References
- Clinical trials for Covid-19: can we better use the window of opportunity. Eichler et al Clinical Pharmacology and Therapeutics
- ICH E6 Good Clinical Practice
- COVID-19: Developing Drugs and Biological Products for Treatment or Prevention Guidance for Industry (FDA)
- COVID-19: how EMA fast-tracks development support and approval of medicines and vaccines
- MHRA Clinical trials applications for Coronavirus (COVID-19)
- WHO Key criteria for the ethical acceptability of COVID-19 human challenge studies
- COMET Initiative: Core Outcome Measures in Effectiveness Trials
- Biomarker Qualification: Evidentiary Framework Guidance for Industry and FDA Staff
The FPM wishes to thank the following FPM members for their contributions in the development of this guidance:
Dr Stuart Dollow FFPM (lead)
Dr Allyah Abbas-Hanif
Dr Alan Bell FFPM
Dr Flic Gabbay FFPM
Dr Michael Holmes MFPM
Dr Maria Isaac FFPM
Prof Andrew Krentz FFPM
Dr Ian Mills FFPM
Dr Gilles O’Bryan-Tear FFPM
Dr Duncan Richards FFPM
Dr Ivana Vranic FFPM
Prof Penny Ward FFPM
